Description DID
SITE MAP DID : Different DSM-IV Diagnoses : For Survivors : Q & A : Survivors’ Stories :
Formerly called Multiple Personality Disorder, Dissociative Identity Disorder is too frequently misdiagnosed and inappropriately treated. ...... UNDER CONSTRUCTION
These questions ought to be repeated from time to time as patients may initially deny symptoms out of lack of trust, or may not yet be aware of the symptoms as being unusual.
The clinician’s awareness of the ways in which patients describe their symptoms usually quickly unmasks the rare case of factitious “DID”.
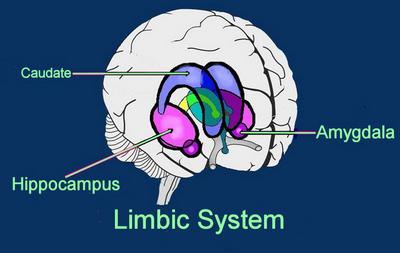
The limbic system is the emotion and emotional memory area, and is part of the primitive unconscious brain. It comprises paired structures nestled deep to the cerebral hemispheres, the lobes of the neocortex.
For more information see inside "Brain"